How to treat endometritis
Often, as a result of difficult delivery, complicated abortions, infertility, miscarriage, and various gynecological interventions, women are faced with a diagnosis of endometritis. Currently, the vast majority of cases of the disease, with timely treatment, can be successfully treated and completely healed.
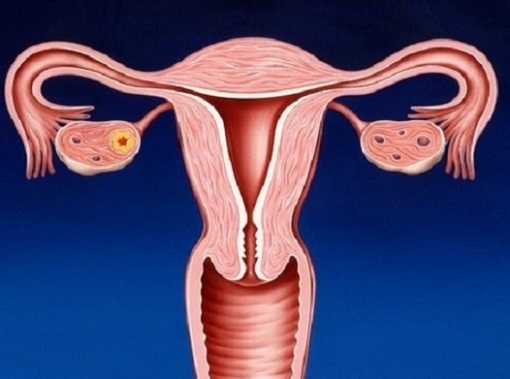
endometritis- inflammation of the inner mucous layer of the body of the uterus (endometrium). The development of inflammation in the endometrium is provoked by viruses and various opportunistic microorganisms: gonococci, E. coli, staphylococci, streptococci, chlamydia and Trichomonas. This disease is quite common and is often accompanied by inflammation of the muscle tissues of the uterus.
Description and types of endometritis
With this disease, the internal mucous membrane in the uterine cavity, which is very important in the functioning of the female body, is affected, its most fragile and sensitive upper layer, the endometrium. There are a lot of factors for the occurrence of the disease, as well as its varieties.
According to the form of manifestation, the disease occurs in:
- Acute, which mainly manifests itself immediately after infection with pathogenic bacteria or pathogenic viruses as a result of mechanical damage and is characterized by severe symptoms.
- Subacute, which can develop as a complication of acute endometritis. As a rule, it occurs in patients with a weak immune system. At this stage, the disease develops into a chronic form. It is urgent to start treatment, because it is the subacute form of E. that can lead to female infertility. During treatment, the doctor prescribes antibiotics, complex preparations from medicinal plants, physiotherapy procedures.
- Chronic (hidden) form. Chronic E. develops as a result of infection with infections that are transmitted through sexual contact. The patient may not be aware of her problem. The disease is often detected after a comprehensive examination for infertility.
According to the etiological principle, all forms of endometritis divided into:
- Specific. This disease, which affects the mucous layer of the uterus, is caused by strictly certain types of microorganisms - tuberculosis bacteria, herpes simplex viruses, pathogens of toxoplasma, mycoplasmas, gonococci, candida, protozoans, cytomegaloviruses, fungal flora. Also, the causative agents of ailments are diseases that are sexually transmitted.
- Nonspecific. All other forms of the disease in the uterine cavity, when it is not possible to detect a specific pathogen of opportunistic microflora, are nonspecific.
Causes of endometritis

The causes of infection of the uterine cavity with various bacteria are quite a large number. Often, minimally invasive diagnostic manipulations become the cause of the disease, so you can catch the disease even while in a medical institution.
Contribute to infection:
- Inaccurate personal hygiene.
- Non-permanent sexual partners. Often, the infection enters the uterine cavity from the vagina during casual sexual intercourse and unprotected intercourse with the carrier of the infection.
- Weakened immune system.
- gynecological interventions. Abortions, therapeutic and diagnostic curettage, probing of the uterine cavity can become a factor in inflammation.
- Hysteroscopy or endoscopic interventions. When carrying out microsurgical manipulation for the purpose of diagnosing, it is also possible to get inflammation of the uterine cavity.
- Mechanical injury to the integrity of the uterus and cervix during childbirth. Sometimes, after the completion of childbirth, the placenta is not born and the doctor has to scrape it out, damaging the inner lining of the uterus.
- Deep postpartum tears in the cervix.
- Dishormonal disorders.
- Associated chronic diseases.
- Establishment of the Navy. Often, after the installation of intrauterine contraceptives, as a result of trauma to the cervix, the inner mucous layer of the uterine body becomes inflamed.
- Physical intimacy during menstruation without protection. Sexual contact during menstruation, even with a healthy partner, can become a factor in the development of endometritis.
- Chronic stress conditions.
The main symptoms of endometritis

The disease in the initial stages can be hidden, without the manifestation of pronounced symptoms, so a woman cannot timely identify endometritis and consult a doctor for treatment. Just this threatens with serious consequences - female infertility, sealing of the walls of the uterine cavity, or the formation of an intrauterine adhesive process. Severe symptoms are characterized by an acute form of endometritis.
Symptoms of manifestation acute endometritis :
- An increase in body temperature up to 38-40 ° C.
- Weak pain in the lower abdomen of a aching or pulling nature, extending to the sacrum or lower back.
- Bleeding from the uterus.
- Changes in the menstrual cycle. They are observed during the transition of the acute form to the chronic form.
- Profuse discharge from the vagina. Cloudy discharge resembling clots and containing blood and pus with an unpleasant characteristic odor.
- Deterioration of general well-being.
Symptoms chronic endometritis :
- Vaginal discharge. With this form, by smell and color, they correspond to the causative agents of the disease. With trichomoniasis, the discharge is abundant and frothy green. With gonorrhea - cloudy yellowish-green mucous discharge.
- Change in the length of the menstrual cycle. Abundant and prolonged periods are observed, more than seven days.
- Smearing discharge at the beginning and after the cycle of menstruation.
- Insignificant or, conversely, abundant discharge during menstruation.
- Repeated spontaneous cases of abortion before the natural term.
- The inability of a woman to conceive a child for a long time (infertility).
- Weak and transient feeling of pain in the lower abdomen.
- An increase in body temperature, often subfebrile, within 37.2 ° C.
Diagnosis of endometritis
At the first visit to the doctor, on the basis of clinical signs and an anamnesis of the disease, a presumptive diagnosis of endometritis is established. At this stage, the doctor asks about all the symptoms that disturb the patient.
In addition to this information, a number of activities and laboratory studies are also being carried out:
- On the gynecological chair, the uterus is examined and the discharge is evaluated by smell, quantity, color.
- Examination of a smear from the vagina for bacterial culture. According to the results of analyzes of bacteriological examination of a smear from the vagina, it is possible to determine with greater accuracy the infectious agent of the disease and its reaction to various medications.
- Sampling and immunohistochemical examination of a vaginal smear. It is carried out to detect infection and the number of leukocytes in a smear.
- Blood test - general analysis.
If necessary, and to establish an accurate diagnosis, additional examinations are carried out:
- Diagnostic intrauterine curettage.
- Histological examination of the endometrium. To confirm the diagnosis of changes in the mucosa (the inner mucous layer of the body of the uterus).
- Ultrasound examination of the uterus and appendages of the female genital organ.
- Endoscopy.
- ELISA blood test for antibodies (ELISA). The study also helps to identify sexually transmitted diseases.
- PCR diagnostics. The polymerase chain reaction is a highly accurate test used to detect numerous specific infections.
This diagnosis of E. is quite enough, however, different diagnostic methods will be carried out at various stages of the disease. Patients with such a disease and in order to avoid the likelihood of developing complications of a septic nature in the form of pelvioperitonitis, peritonitis, undergo treatment in medical institutions in a hospital.
Features of the treatment of endometritis

The treatment regimen for the disease depends on the results of the examination. With well-chosen treatment, this disease can be completely healed in a week, and women who are faced with an illness will have a chance to become pregnant and give birth to completely healthy babies. As a rule, treatment is carried out with broad-spectrum antibiotics.
For successful treatment, drug treatment is used in combination with physiotherapy, vitamins and agents that improve microcirculation, if necessary, hormonal drugs are prescribed. As an addition to traditional therapy prescribed by a gynecologist, traditional medicine is used in timely treatment.
Treatment of endometritis with drugs.

A qualified doctor in the treatment of E., first of all, prescribes antibiotics, which can relieve inflammation and reduce discharge. In addition, antibiotic therapy, which is best performed in the early stages of the detection and course of the disease. Patients are often prescribed protected drugs.
With a not very severe course of the disease, the doctor may prescribe antibiotics, in which the woman can even continue breastfeeding the baby. With a pronounced pathology, breastfeeding will still have to be abandoned and treated with the strongest antibiotics.
Drugs, as a rule, are prescribed in the form of tablets, administered as droppers or intravenous injections, as well as local remedies to get rid of itching, burning sensation in the vaginal area.
In addition to antibiotics, an experienced doctor can prescribe the use of antifungal drugs in parallel.
The main medications in the treatment of endometritis:
- Antispasmodics. A group of drugs that relieve painful attacks of spasmodic pain. In a hospital setting, the patient is administered pr-you twice a day. Medicines reduce pain irritation in the lower abdomen and in the sacral spine.
- Antibiotics. In the early stages of the development of the disease, antibiotics of a diverse spectrum of effects are prescribed. In a medical institution, these drugs are administered in the form of injections. When treated at home, they are prescribed in tablet form.
- Antifungal medicines. If necessary, the appointment of antibiotics is combined with the simultaneous administration of antifungal drugs, due to the possible risk of developing candidiasis.
- Antipyretic. Such drugs are prescribed in the case when the patient has an elevated body temperature.
- Means that relieve swelling of the mucous membrane. To block histamine in the body, fairly effective and safe decongestants are prescribed. These drugs help to reduce the size of the uterus, relieve the inflammatory process and swelling of the tissues.
Treatment of endometritis with topical medications

If the disease was provoked by an infection that is transmitted through sexual contact, in this case, in addition to antibiotics, the doctor prescribes topical drugs. Candles and medicinal substances in the form of suppositories help to quickly get rid of secretions and destroy pathogenic microorganisms right at the source of infection.
Candles and ointments used in the treatment of endometritis:
- Preparations with the active substance - chlorhexidine, whose action is aimed at combating bacteria, viruses and fungal diseases. Effectively used in the treatment of endometritis caused by microorganisms of the genus Trichomonas, opportunistic bacteria gardnerella and chlamydia. Medicines in the form of suppositories are placed twice a day. Morning and evening before bed.
- Combined candles, universal action. These drugs are effective against pyogenic bacteria, fungi of the genus Candida, microorganisms of the genus Trichomonas and Gram (+) bacteria. Such a wide variety of actions of drugs is due to the substances contained in the composition of suppositories. To cure E. drugs put two r / day for ten days.
- Drugs prescribed after ultrasound examination and confirmation of the presence of adhesions and a strong inflammatory process in the uterine cavity. The drugs have an antioxidant, pronounced immunomodulatory, anti-inflammatory effect. Thanks to the components that make up the preparations, the swelling of the uterus decreases and adhesions are destroyed.
- Combined vaginal capsules. The candles contain antimicrobial and antifungal substances. The main advantage of the pr-that is that its components do not cause a violation of the beneficial microflora of the vagina. Candles are used for E. caused by Gram (+) and Gram (-) microorganisms.
- Vaginal suppositories, actively used in gynecological practice. Thanks to the substances contained in their composition, the drug has a pronounced antimicrobial, antifungal, antiprotozoal effect, and also helps to accelerate the formation of the stratum corneum. The drug is used in the treatment of acute and chronic forms of E., the causative agent of which are infections transmitted through sexual intercourse.
- Candles containing iodine in its composition, which has a depressing effect on the growth and reproduction of pathogenic and opportunistic microorganisms. The drug is characterized by antiseptic, antifungal, disinfectant and antiprotozoal effect, has a wide spectrum of antimicrobial activity. The medicine is effective in E., the development of which was provoked by a fungus, viruses and bacteria (including Staphylococcus aureus and E. coli), as well as protozoa.
Physiotherapy for endometritis

With E., for a therapeutic effect on some organs or on the whole organism, the use of physiotherapy is an important component of treatment, because it helps to improve the conduction of drug therapy and the patient's rapid recovery.
Physiotherapeutic methods of treatment are prescribed to reduce pain (analgesic methods), relieve inflammation in the uterine mucosa and restore the structure of the endometrium (reparative-regenerative methods), activate local immunity (immunostimulating methods methods).
Physical methods of treatment of patients with endometritis:
- UHF therapy. Anti-exudative technique with the impact on the body of a high-frequency electromagnetic field and helps to reduce the inflammatory process.
- Reparative-regenerative methods. The method involves procedures using laser therapy with infrared radiation on the projection area of the uterus, paraffin therapy - using medical paraffin, iodine-bromine baths, radon baths, hydrogen sulfide, and pelotherapy procedures - limit the release of fluid and swelling of tissues, promote the development of connective tissue and treatment with ozokerite therapy.
- Analgesic method - ultraviolet irradiation (UVR). Medium-wave ultraviolet irradiation in erythemal doses. UVI of the vaginal mucosa leads to the death of most pathogenic microorganisms. The method will be especially effective if the cause of the disease is vaginosis.
- Immunostimulating methods: LOK-therapy, heliotherapy, thalassotherapy treatment, suberythemal doses of UV radiation, treatment with air baths.
- interference therapy. The essence of the method is the impact on the human body of two currents of medium frequency, which form the so-called interference low-frequency current, while having a positive effect on tissues. This therapy raises the pain threshold and due to this, subjective pain irritation disappears.
- Laser therapy. Exposure of the tissues of the mucous layer of the uterus to radiation of light waves of a certain length increases local immunity, improves microcirculation and promotes the rapid healing of damaged tissues. Laser radiation also has a certain bactericidal effect, causing the death of pathogenic microorganisms.
- Magnetotherapy. The method of alternative medicine using the influence of a magnetic field on the human body reduces the inflammatory process and swelling, improves microcirculation, increases metabolic processes in the mucous layer of the uterus, contributing to the rapid healing and restoration of damaged tissue. In addition, local immunity and other cells of the immune system are activated, the defenses of the female body are increased.
- Ultrasound therapy (UZT). The impact of ultrasound with a certain frequency causes a number of changes in the tissues of the body, contributing to the activation and acceleration of metabolism. It also improves microcirculation and tissue trophism, loosens the connective tissue, which prevents the formation of adhesions.
- Electrophoresis. The treatment procedure is aimed at the penetration of the drug deep into the tissues under the influence of an electric current using copper, iodine, zinc, 10% calcium iodide solution for the treatment of pain.
With relative harmlessness, physiotherapeutic procedures still have some contraindications that should be considered when prescribing.
The use of physiotherapy treatment of endometritis is absolutely contraindicated in:
- acute period of the disease;
- purulent E. (metroendometritis);
- pelvioperitonitis;
- during pregnancy;
- uterine bleeding;
- neoplasms (tumors in the affected area);
- polycystic ovaries;
- with the growth of the inner mucous layer of the uterine body (endometrium) outside the uterine cavity.
In other cases, the use of physiotherapy treatment is decided by the attending gynecologist and physiotherapist.
Hormonal treatment
In view of the fact that the cause of inflammation of the inner functional lining of the uterus can be not only infections and bacteria, but also a violation in the development and rejection of the mucosal layer, the attending physician may prescribe hormonal drugs for three to six months (usually oral contraceptives) .
Taking combined oral contraceptives helps to restore the menstrual cycle, and after stopping taking OK in a woman against the background of the so-called withdrawal syndrome of birth control pills, pregnancy can often occur.
Treatment with folk remedies

When treating E., gynecologists often prescribe traditional medicine to eliminate vaginal discharge. However, it should be remembered that if this disease was caused by sufficiently dangerous microorganisms and viruses, then it will not be possible to cure endometritis without special assistance and taking medications.
Under O.E. you can not use treatment only with traditional medicine. Traditional medicine for the treatment of the disease offers douching with infusions or decoctions of medicinal herbs.
Recipes of traditional healers:
- Herb coltsfoot. The tannins contained in the plant have a pronounced antibacterial and anti-inflammatory effect. To prepare a decoction, pour 50 grams of crushed raw materials with one liter of boiling water and insist for four hours. After that, strain and take one tablespoon four to five r / day.
- Bay leaf. For the treatment procedure, 20 grams of dry raw materials will be required. Pour the plant into a deep enameled container, pour water and boil for about five minutes. Let the broth cool a little and sit down on a bucket, wrapped in a terry sheet. The procedure is carried out before going to bed for two weeks. The decoction is excellent for inflammation of the genitourinary system.
- Nettle leaves. The plant suppresses the inflammatory process, has an antimicrobial effect, stimulates the metabolism in the body and improves the contractile activity of the muscular walls of the uterus (myometrium). To prepare the medicine, pour one tablespoon of crushed raw materials with one liter of boiling water and insist for three hours. Strain the broth and take one tablespoon of the broth four r / day 30 minutes before meals and at bedtime.
- Sea buckthorn oil. This is an old and quite effective way. It is necessary to soak a cotton swab wrapped in a sterile bandage with sea buckthorn oil. Put a tampon on at night. The duration of treatment is two weeks. The oil relieves the inflammatory process and helps scar tissue of the cervix.
- St. John's wort herb. To prepare a decoction, you need to pour 20 grams of dry raw materials on the floor with a liter of boiling water and simmer for about ten minutes over low heat. Strain the finished product and take three r / day for 1/2 tbsp.
- Blueberries. A decoction of the berries of the plant inhibits the development of inflammation, has an astringent, antimicrobial and slight diuretic effect. To prepare the drug, pour one hundred grams of dried berries of the plant with one liter of cold water, bring to a boil and boil for ten minutes. Cool the broth and consume 1/2 tbsp. (100 milliliters) 3 r / day.
- Forest hay. It is necessary to place a bunch of hay in a bucket and pour five liters of water. Bring to a boil and remove from heat. Sit the patient on a bucket and wrap yourself in a blanket. It is necessary to sit until the broth cools. The duration of treatment is two weeks.
- Dried fern leaves. It is necessary to pour 20 grams of raw materials with 280 milliliters of cold water and boil for two minutes. Strain the finished broth and consume 70 milliliters three to four r / day. The duration of treatment is two weeks.
- Citrus fruits. Wash well and dry thoroughly, one large orange and one lemon each. Grind tropical fruits in a blender or twist in a meat grinder. Enter ten caps into the resulting mass. onion juice and 10 grams of sugar. Cover the jar with a lid and shake well. Take the drug one teaspoon three to four times a day. The duration of treatment is three weeks.
Endometritis and pregnancy, after childbirth

It is impossible to get pregnant with endometritis, endure a normal pregnancy and give birth to a healthy child. Moreover, if the disease is not cured in a timely manner, then the developed pathology can lead to incurable infertility. With the development of E., the complex processes of conception and implantation of the embryo into the mucous membrane that covers the inner surface of the uterus are disrupted, and this makes the mechanism of development and bearing of the fetus impossible.
During pregnancy This disease is one of the most dangerous, so you can not be irresponsible about this problem. At the first signs of the manifestation of the disease, you should immediately consult a doctor and take endometrial scrapings for analysis. If the diagnosis is confirmed, it is necessary to immediately begin treatment, and if the doctor prescribes antibiotic therapy, one should not refuse, otherwise, as the disease develops, the consequences can be extremely deplorable - the fetus will die.
To increase the chances of a successful conception, in the future you need to undergo a course of treatment with hormonal therapy, which will have a beneficial effect on the normal course of pregnancy.
E. after childbirth is a frequent complication after a difficult delivery, and, as a rule, is diagnosed using ultrasound.
The causes of postpartum E. consider:
- Complication of a normally developing pregnancy (preeclampsia).
- A protracted birth period, especially if the child has been without amniotic fluid for a long time.
- The birth of a large baby, the wrong presentation of the fetus.
- Narrow birth canals.
- Childbirth in a woman, after the forty-first child.
- Childbirth at an early age - up to nineteen years.
- Detachment of the placenta prematurely.
- Infection of the mother with an STD.
Is it possible to have sex with endometritis?

It is not recommended to have intimate relationships with endometritis, because this can not only provoke a complication during the course of the disease, but also cause infection of the sexual partner. During sexual intercourse, the integrity of the mucous plug secreted by numerous glands is violated - a barrier that blocks the entrance to the uterine cavity and prevents infection of this area from the external genital organs and the environment. If you do not use a mechanical means of protection (a condom), an infection from an unhealthy partner can enter the uterus and cause E..
Intimacy with endometritis can be complicated:

- The spread of microbial infection to neighboring organs and throughout the body.
- The occurrence of adhesions and nodes in the fallopian tubes leads to infertility. This creates an obstacle to the movement of the egg to the uterus and makes it impossible to get pregnant and carry the baby normally.
- The appearance of polyps in the uterus.
- Germination of the mucosal layer into the muscular tissue of the uterus (myometrium) and beyond the uterine mucosa, directly into the abdominal cavity. With adenomyosis, scars form in the uterus that prevent the conception of a child. In addition, spotting is constantly observed, as well as pain during sexual contact.
- Cysts form. Constant inflammation leads to the formation of a benign neoplasm in the uterus or on the ovaries.
- The risk of miscarriage (miscarriage) in the early stages and the likelihood of premature birth.
- Failures of the cycle of menstruation.
Prevention of endometritis

Preventive measures of this disease are aimed at eliminating the factors predisposing the occurrence of the inflammatory process and the penetration of pathogenic microorganisms into the uterine cavity, and if this still happened, to eliminate them as soon as possible.
Measures to prevent endometritis include:
- Timely treatment of infections transmitted through sexual intercourse.
- Treatment of complications that occur during childbirth.
- Refusal of artificial termination of pregnancy (abortion).
- Regular passage of gynecological examinations and the study of the microflora of the woman's vagina after childbirth and before medical procedures.
- Attentive attitude of a woman to herself: observance of personal hygiene of the genital organs, in time to contact a qualified obstetrician-gynecologist.
- Lead a healthy lifestyle (healthy lifestyle), engage in disease prevention and improve health.
- Use of condoms during sexual intercourse.
- Strengthen the immune system.
- Intercostal neuralgia - what is it and how to treat
- How to quickly get rid of dry corns on the legs
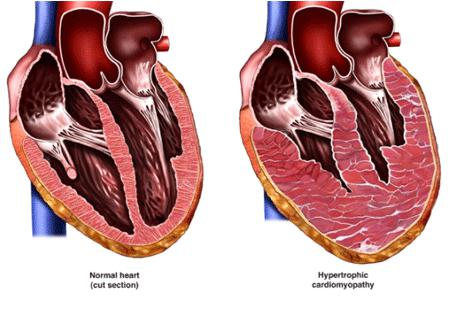
- How to treat left ventricular hypertrophy
- Rating of the best drugs for rotavirus for children
- Making tea from currant leaves, the benefits and harms of the drink
- How to drink hydrogen peroxide according to Neumyvakin - an oral regimen
- Features of the treatment of plantar fasciitis with folk remedies
- The composition and beneficial properties of parsley root
- How to get pregnant quickly? Folk remedies
- Herbs-ants in the "pot-bellied" period or the use of herbal medicine during pregnancy
- Why does a sore throat and dry cough occur, and what treatment is required?
- Guy's Room Design: Ideas and Examples
- General rules for drawing up a foundation plan House foundation drawings
- modern art deco bedroom small art deco bedroom
- Pansies: characteristics and photos of flowers
- Making an art deco bedroom: the choice of materials Beige art deco bedroom
- Bedroom interiors in art deco style Bedroom art deco style beige
- Young: planting and care in the open field Young planting and care in the open
- Varieties for open ground
- Pansies: cultivation and care in the open field